The Problem
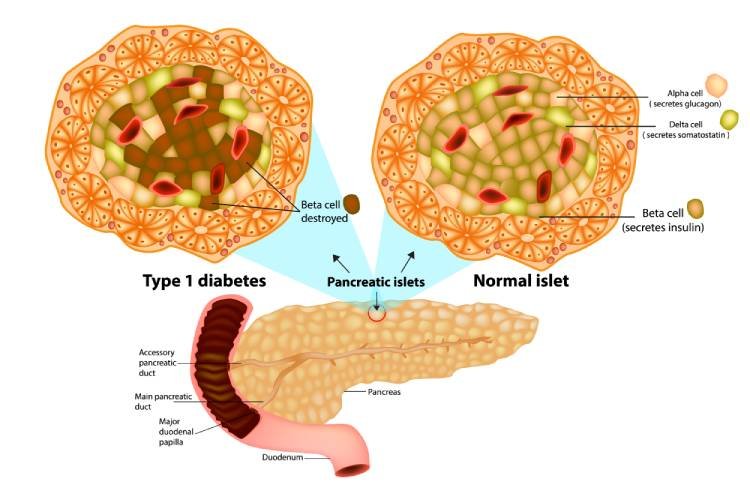
Type-1 Diabetes Mellitus is an autoimmune disorder where the immune system mistakenly attacks insulin producing beta cells in the islets of the pancreas. After a significant portion of these insulin-producing cells have been destroyed, the pancreas is no longer able to produce enough insulin for the body. The standard treatment for this disease is daily glucose monitoring and insulin injection. Unfortunately, even with rigorous insulin therapy, many complications eventually arise for those suffering from insulin dependent diabetes including multi-organ failure (kidneys, heart, eyes, nerves, etc.), vascular complications including amputations and stroke, visual issues leading to blindness, and an early death. Alternative therapies, including pancreas and islet cell transplants from unrelated donors are not practical due to the large number of donors needed (up to five donors for a single treatment, and at least two treatments are needed) to provide freedom from exogenous insulin. In addition, the requirement for administration of immunosuppressive agents in transplant recipients is often associated with the development of serious infections, cancers, and kidney disease.
The Solution
Durable Stem Cell-based Biologic Therapy: “Neo-Islets.”
Depicted here, our patented biotechnology utilizes both allogeneic Pancreatic Beta Cells and Mesenchymal Stem Cells (MSC) engineered into hybrid clusters that engraft in the omentum and provide physiologic insulin secretion and achieve euglycemia in the host.
SymbioCellTech Technology
SymbioCellTech (SCT) has developed and patented the technology for a fundamentally new adult stem cell-enabled therapy in which culture-expanded insulin expressing cells are combined with high numbers of Mesenchymal Stem Cells (MSCs) to form unique three-dimensional geometric cellular clusters we call "Neo-Islets." When administered into the abdominal cavity Neo-Islets not only establish a new source of physiologically regulated insulin to the bloodstream but also provide the critical benefit of immune isolation from destructive immunosurveillance.
Diabetes researchers have struggled for many years to create islet encapsulation devices to protect against the immune-attack problem in Type-1 diabetes. These devices tend to fail due to foreign body reactions. SCT invented Neo-Islets as a way to provide "natural encapsulation' rather than using a foreign medical device.
The technical details and data in support of SCT's Neo-Islet technology are more fully described in a recent publication in the journal Stem Cells Translational Medicine. Our Neo-Islets were featured on the cover of the July 2017 issue. The article can be found here. A PDF version of the publication can be downloaded here.
SCT’s Neo-Islets have been shown in preclinical studies to functionally cure Type-1 diabetes. Studies are also underway to address Type-2 diabetes. This therapy can be administered in a simple out-patient procedure, and treatment is expected to last a lifetime. A clinical trial in diabetic pet dogs has yielded promising results, with an up to 50% reduction in the need for insulin and a simultaneous reduction in blood glucose levels of ~100mg/dL, both sustained for over 15 months thus far. SCT is aiming to begin Phase I, human clinical trials in 2023.
Neo-islets Overcome multiple Technical Obstacles
There are four major technical challenges faced by cell-based diabetes therapies.
Immune Attach
Cellular therapies face two immune challenges. First, the immune system of a Type-1 diabetic attacks and destroys insulin-producing pancreatic β islet cells, and this autoimmune attack must be overcome. Second, any newly transplanted pancreatic islets or insulin-producing cells from an unrelated donor would be seen as “foreign” and must be protected from what is called an allo-immune attack. This challenge would be faced by any cellular therapeutic for Type-2 diabetics, too. Both of these types of attacks can be stopped through the use of immunosuppression drugs, but these can have severe side-effects and should ideally be avoided. As is shown in our published work, and as we have found from our pilot study in pet dogs, the stem cell component of SCT’s Neo-Islets shields the insulin-producing cells within them from either type of immune mediated destruction, allowing them to survive long term and produce insulin as needed.
Donor Scarcity
Physiologically competent islets or insulin-producing cells are difficult to culture, grow, or mass produce in a lab, and several organ donors are needed to produced enough islets for a single patient. The scarcity of donors limits the ability to produce sufficient numbers of islets for worldwide islet transplant therapy. A viable cure for diabetes must provide a way to produce mass quantities of insulin-producing cells from a relatively small number of pancreas donors. Based on preclinical tests, we estimate that approximately 80 doses of human Neo-Islets can be created from a single pancreas donor, and further optimization of our methods could increase this yield.
Vascularization
New blood vessels must be formed and connect to transplanted islets for long-term survival in the body. Without neo-vascularization insulin-producing cells die from inadequate blood supply, nutrients, oxygen, and energy stores. The stem cell component of SCT’s Neo-Islets protect and nurture beta cells and promote the creation of new blood vessels to provide a direct supply of nutrients through the blood stream.
Physiologic Insulin Delivery
In a healthy individual, insulin is released by the pancreas directly into the portal system of the liver. This is the most natural, safe and effective means for insulin delivery. The traditional therapy of injecting insulin under the skin, and the approach of implanting cells contained within encapsulation devices sub-cutaneously are both sub-optimal. Sub-cutaneous insulin delivery results in poor glucose control and exposes local tissues and organs to potentially harmful levels of insulin. To further complicate matters, proper insulin delivery is highly dependent on effective glucose sensing which cannot be reliably performed from locations in the skin or within encapsulation devices. SCT’s technology solves the insulin delivery problem by releasing insulin from Neo-Islets housed in the omentum. Like that of the pancreas, the blood supply of the omentum goes directly into the portal system of the liver.